Volume 2 Issue 5 May, 2012
Alcohol Withdrawal features are commonly encountered in clinical practice across specialties and most of the time the patient may not have revealed to the clinician that he consumes alcohol regularly or has problem drinking. Criteria to say person is in withdrawal state are, there should be reduction or cessation of alcohol use following which there must be two or more of the symptoms like, insomnia, hand tremor, tachycardia, sweating, nausea, vomiting, transient visual auditory or tactile hallucinations, psychomotor agitation and seizures, causing significant distress or impairment in social & occupational functioning. Withdrawal symptoms can occur in any settings for example patient admitted in medical, surgical or orthopedic ward etc. Symptoms of withdrawal relate proportionately to the amount & duration of alcohol intake, & also recent drinking habit.
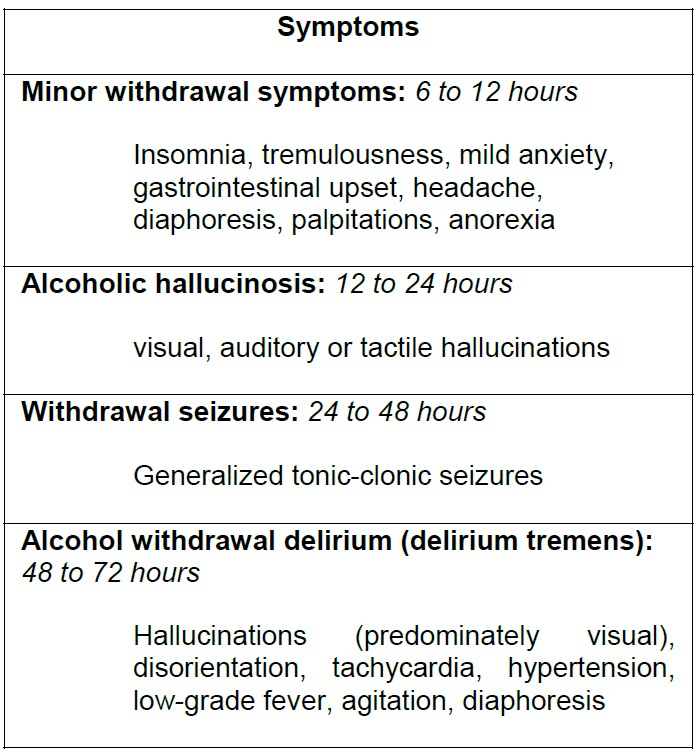
The spectrum and time range for the appearance of symptoms after cessation of alcohol use are listed below.
Management of alcohol withdrawal
General care: Never over look physical condition. Supportive care like correction of fluid level, electrolytes or nutrition should be taken care. Multivitamins and thiamine100mg per day should be given before the glucose is administered to prevent precipitation of Wernicke’s encephalopathy.
Pharmacological management: Detoxification is the medical management of withdrawal symptoms. Medications can be fixed schedule or symptom triggered regimen. Benzodiazepines have been shown to be safe & effective particularly for preventing or treating seizures and delirium. Important note that there is no antiepileptic prophylaxis is required for alcohol withdrawal seizures.
Choice of the agent should be based on pharmacokinetics.
Diazepam & Chlordiazepoxide are long acting & excellent, because of the long half life, withdrawal is smoother & rebound withdrawal symptoms are less likely to occur. Lorazepam and oxazepam are intermediate acting may be preferable in patients with liver failure and elderly.
Fixed schedule therapy: Predetermined amount of drug in divided doses over the day on day 1 dose, then gradually tapered off over 7 to 10 days.
One unit standard drink = 10 gms of ethanol requires = 10 mg of chlordiazepoxide = 5mg of diazepam = 1mg of lorazepam
One standard drink = 30ml of spirit (whiskey, rum, brandy, gin) = 60ml of wine = half bottle of beer = 1/3rd sachet of arrack
Choice of treatment setting: With mild to moderate withdrawal symptoms, outpatient detoxification is safe and effective, however severe withdrawal symptoms, history of withdrawal seizures or delirium tremens, multiple previous treatment failures, concomitant psychiatric or medical illness requires inpatient care.
Management of alcohol withdrawal syndrome should be tailored in each case & should be followed by deaddiction treatment for alcohol dependence.

Mandya Institute of Medical Science
